Researchers first to unlock key molecular mystery of premature aging syndromes
Florida State to conduct breakthrough research on premature aging diseases called “progeroid syndromes.”
New research from Florida State University is beginning to piece together the stubborn puzzle posed by a family of rare and debilitating premature aging disorders.
Most of these diseases, called progeroid syndromes, share physiological symptoms characterized by the appearance of accelerated aging, such as skin disorders, loss of hair, skeletal and dental abnormalities and cardiovascular complications. Each individual progeroid syndrome is caused by its own specific genetic mutation, but researchers have struggled to describe what these different diseases have in common. This persistent mystery has limited scientists’ exploration of potential therapies or treatments.
In a pioneering study published this week in the journal Proceedings of the National Academy of Sciences, FSU researchers outlined the first discovery of a molecular commonality between two progeroid syndromes, Hutchinson-Gilford progeria syndrome and Rothmund-Thomson syndrome, and introduced a method for disease recognition that could yield additional breakthroughs in the future.
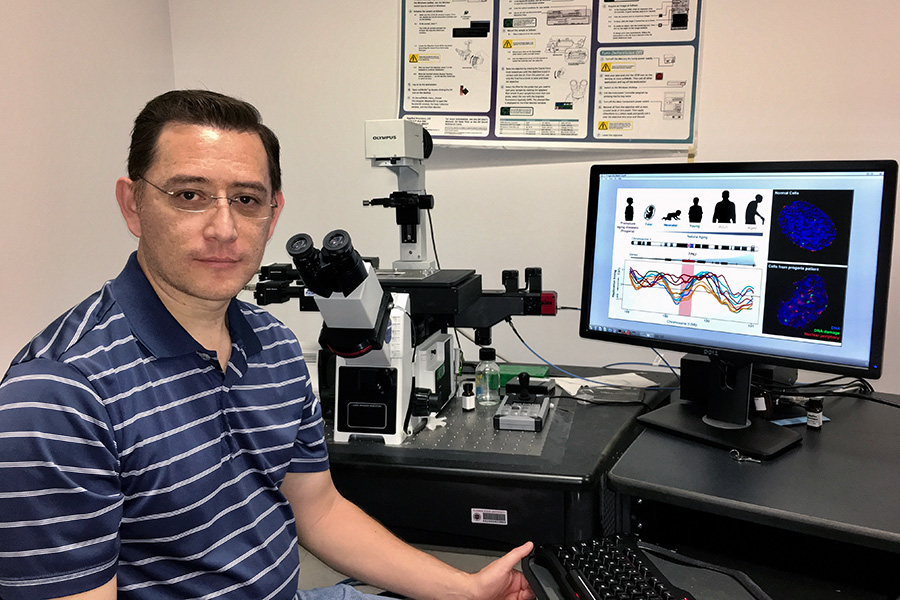
“There are many different individual mutations that can cause progeroid diseases, but nobody has been able to find any specific common quality between them,” said postdoctoral researcher Juan Carlos Rivera-Mulia, the lead author of the study. “This research is the first discovery of a molecular commonality between two progeroid diseases with two different genetic causes.”
In popular culture, notions of premature aging syndromes are typically expressed in the stories of fanciful characters like Benjamin Button, who ages backward out of his frail condition and emerges as a strapping, healthy middle-aged man. For the people who suffer from these diseases in the real world, life looks radically different.
In Hutchinson-Gilford progeria, children as young as 1 to 2 start developing a host of dramatic symptoms, and they die at an average age of 14. In Rothmund-Thomson syndrome, symptoms develop during childhood, and although life expectancy is not affected as dramatically, patients are predisposed to develop cancer. Progeroid syndromes are rare — one in 4 million newborns worldwide are diagnosed with Hutchinson-Gilford and there are 400 documented cases of Rothmund-Thomson — but there are no existing treatments or workable therapies for these diseases.
To better understand the underlying molecular mechanics of these disorders, researchers employed an advanced approach to disease marker discovery developed and refined at Florida State.
This method, called “DNA replication timing profiling,” involves monitoring the order in which segments of DNA are duplicated in preparation for cell division.
Before a cell divides, it has to duplicate the roughly 15,000 chromosomal segments that compose its genome. This replication process is rigidly ordered, and cells originating from different tissues in the body have different timelines of DNA segment replication. DNA in skin cells, for example, will have a different replication timing profile from DNA in cardiovascular cells

J. Herbert Taylor
Distinguished
Professor of Biology
In many diseases, this highly regulated and programmatic replication timing becomes disrupted. FSU researchers have found that characterization of these disruptions can reveal the fundamental molecular misfirings that give rise to different genetic disorders.
“We’d been studying the mechanism of how this replication process is regulated, and we’d been trying to understand why the process is regulated differently in different cell types,” said the J. Herbert Taylor Distinguished Professor of Biology David Gilbert, the senior author of the paper. “In the course of those studies, we recognized that this methodology could be very useful for the study of diseases like leukemia, and we’ve already used the system to identify alterations that can classify different leukemia subtypes.”
For this study, Rivera-Mulia and his colleagues collected cells from progeroid patients and converted them to pluripotent stem cells, allowing for a reliable model of human development. Researchers found that all abnormalities were erased when the cells were modified to stem cells, but when they were converted back into skin cells, the progeroid-related abnormalities gradually began to reemerge.
One early abnormality, an alteration in the gene TP63, was found to appear in both Hutchinson-Gilford and Rothmund-Thomson syndromes.
Not only was this the first time anyone had identified a molecular commonality between two progeroid syndromes — a monumental breakthrough in the study of these conditions — but it was also a resounding endorsement of the replication timing method’s utility as an epigenetic tool for detecting markers of disease.
“This was more than just a discovery in progeroid disease,” Gilbert said. “This was the first novel finding using replication timing as a biomarker. We’ve shown we can find really interesting things with this method in leukemia, but until now, we’d yet to hit on something truly new. It’s a pretty significant discovery.”
The next step, Rivera-Mulia said, is to continue using reprogrammed stem cells to explore the development of progeroid syndromes in cell types that are most affected by these diseases and to trace the misregulations or abnormalities that occur during those processes.
If researchers can continue to map the molecular connections between these various premature aging diseases, the hope of finding a cure is not out of the question.
“We first need to identify the commonalities between these diseases and how they relate to natural and premature aging,” Rivera-Mulia said. “If we can find the mechanistic causes of the alterations in these genes, and we can develop a targeted therapy, there’s a chance we can one day find a cure.”
This research was funded by the National Institutes of Health, the French Ministry of Research and the Centre National de la Recherche Scientifique in Paris. FSU researchers Claudia Trevilla-Garcia, Takayo Sasaki, Jiao Sima and Tyler Fells also contributed to this study. Other collaborators include Romain Desprat, Hélène Schwerer and Jean-Marc Lemaitre from the Laboratory of Genome and Stem Cell Plasticity in Development and Aging at the Université de Montpellier in France and Daniela Cornacchia and Lorenz Studer from the Center for Stem Cell Biology at the Sloan-Kettering Institute in New York.

